Legg-Calvé-Perthes disease occurs when part or all of the ball of the hip (femoral head) loses blood supply. Without adequate blood flow, the bone weakens and can collapse leading to deformity of the hip. The cause of Perthes disease is currently unknown. Perthes disease is not genetic or hereditary in most cases since less than five percent of children with the disease have a family history of the disorder. There are hip conditions that are inherited that can mimic Perthes disease, such as multiple epiphyseal dysplasia and other skeletal dysplasia.
Perthes disease is a diagnosis of exclusion, which means that because there are other conditions that can mimic Perthes disease, similar conditions must be ruled out by taking a careful medical history and doing a thorough physical examination. Physicians generally ask about family history of hip disorders, family history of early joint replacement, previous hip surgery, past use of steroid medication for asthma or other medical conditions, history of sickle cell disease, history of hip infection, clotting disorders and endocrine disorders. In children, a hip disorder can elicit knee or thigh pain thus careful examination is required to correctly localize the anatomic location of the problem.
In addition to medical history and physical examination, X-rays of the hips are required to make the diagnosis of Perthes. In a small number of patients who come to the clinic shortly after the onset of symptoms, the X-rays may be normal if not enough time has passed for changes to occur. If the patient is still suspected of having Perthes disease, a perfusion MRI may be helpful to make the diagnosis, as it is more sensitive than conventional MRI.
Various treatment methods exist for Perthes disease, and the best treatment option depends on several factors, such as the age of the child at onset of the disease, the amount of femoral head involvement and the stage of the disease at diagnosis. Because of these factors, plus the child’s ability to comply with treatment instructions and a doctor’s findings during examination, treatment is individualized. No single treatment method will work for all patients, and no single treatment consistently prevents the development of femoral head deformity.
The primary treatment goals are to alleviate pain and to prevent lasting deformity of the femoral head. Because it is easier to prevent or minimize femoral head deformity than to restore the round shape of the femoral head after it has flattened or collapsed, early institution of treatment is important for older patients (8+ years) who do not have good femoral head reshaping potential. Treatments that restore hip motion and help reshape the femoral head as best as possible are used when the child is diagnosed at a later stage of the disease.
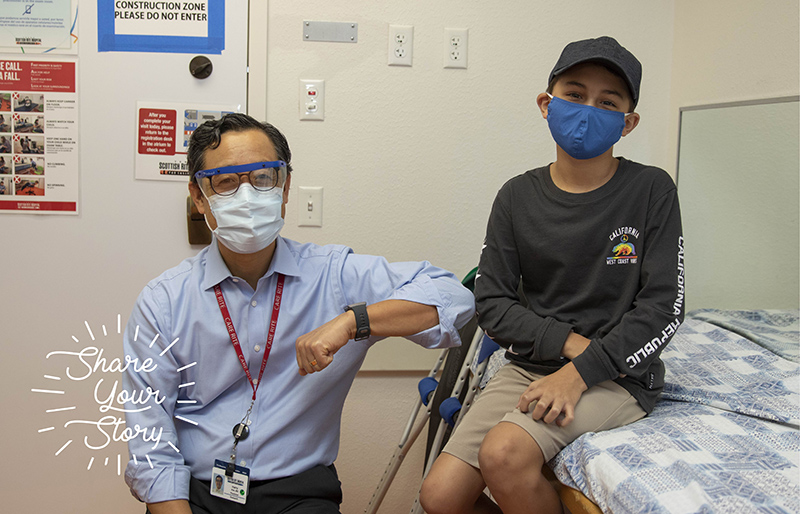
We would recommend a consultation with your physician to determine the activities that are safe and beneficial because the answer would depend on the stage of the disease, your child's symptoms, hip joint stiffness and your child's age.
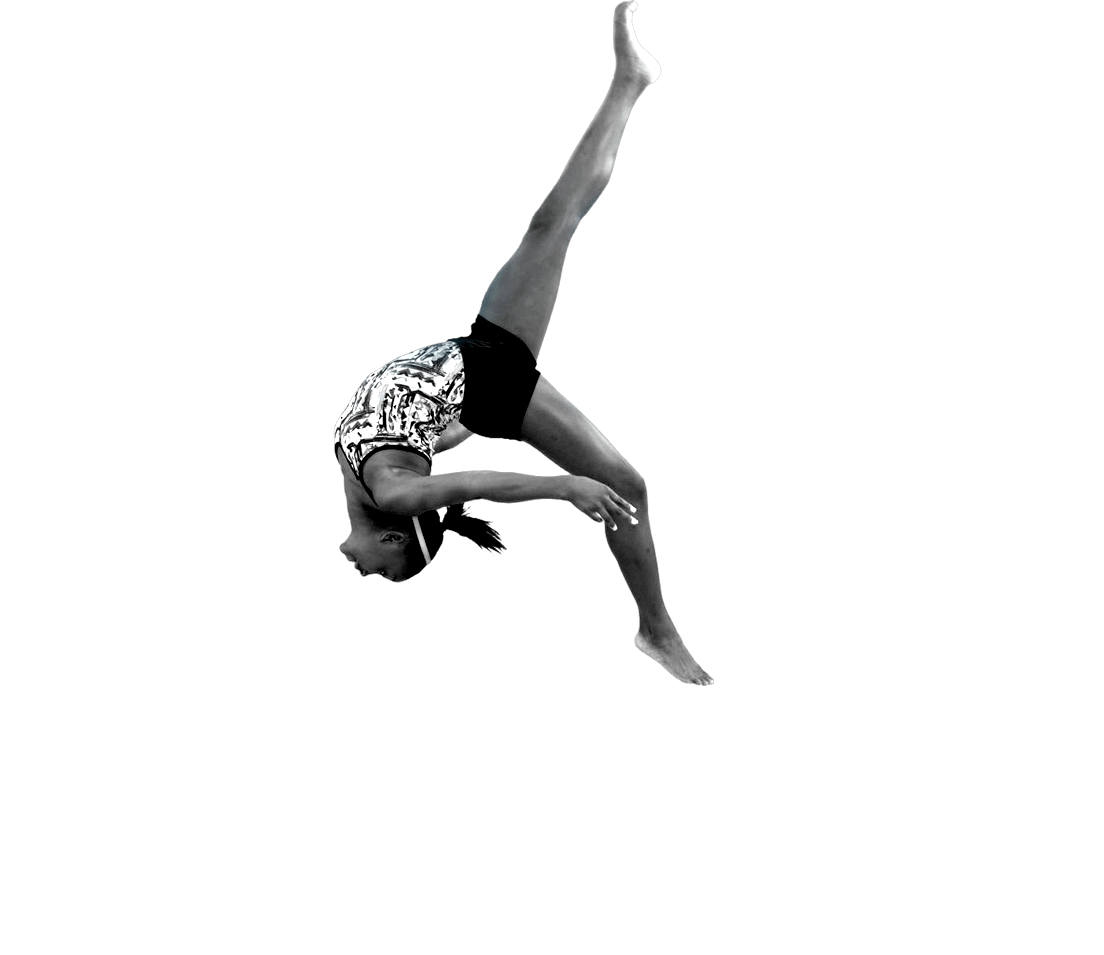
In our experience, most patients are able to return to running and sports once the femoral head is in the late re-ossification or healed stage.
It is a disease because it adversely affects the cells in the femoral head and affects hip function and development.
Pain generally suggests that there is hip joint inflammation and your child may be doing too much activity that irritates the inflammation. The amount of pain experienced by a child with Perthes disease varies from patient to patient. Some patients complain of activity-related pain or night pain only. Your child may complain of groin, thigh or knee pain. They may have restricted movement and a mild to noticeable limp. You and your child’s doctor will discuss how to best manage pain.
Although the blood flow to a part or all of the femoral head is disrupted and stops the femoral head from growing, a return of blood flow and healing will occur over time since tissue around the affected femoral head is alive and is able to respond to the abnormal change. In many patients, especially those with early onset of the disease (before age 6), normal growth is restored as the new vessels enter the dead bone and start the healing process. In older patients, restoration of normal growth of the hip is not as predictable.
Hip replacement is not a surgery for children. Only if a patient develops painful degenerative arthritis later in adulthood is the hip replacement surgery warranted. Even with a deformed femoral head, most patients can perform daily activities and sports activities once the hip has healed.
It is not curable because we don't know the cause. However, it is a self-healing disease, meaning the body is able to heal the bone in the femoral head that is affected. The healing process and the duration of the disease vary from patient to patient. The clinical outcome also varies, depending on the age of the patient, the extent of femoral head involvement and the amount of femoral head collapse.